SKULL BASE CANCER CANCER CANCER
SKULL BASE CANCER CANCER CANCER
What is SKULL BASE cancer?
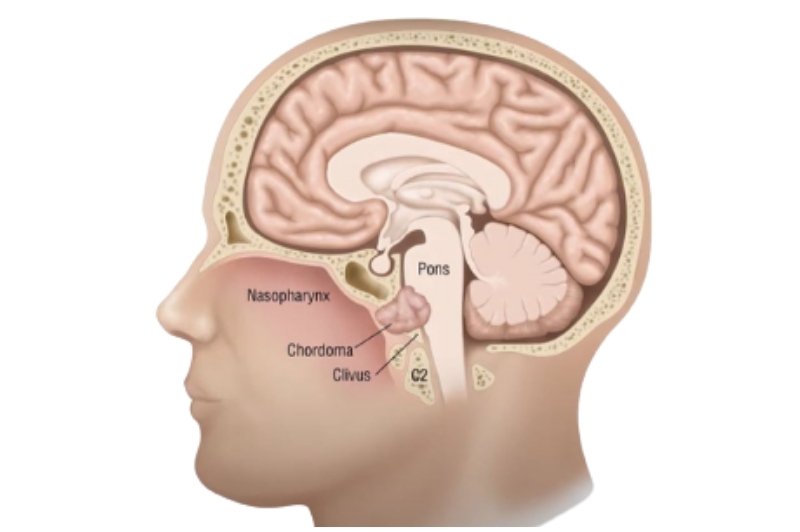
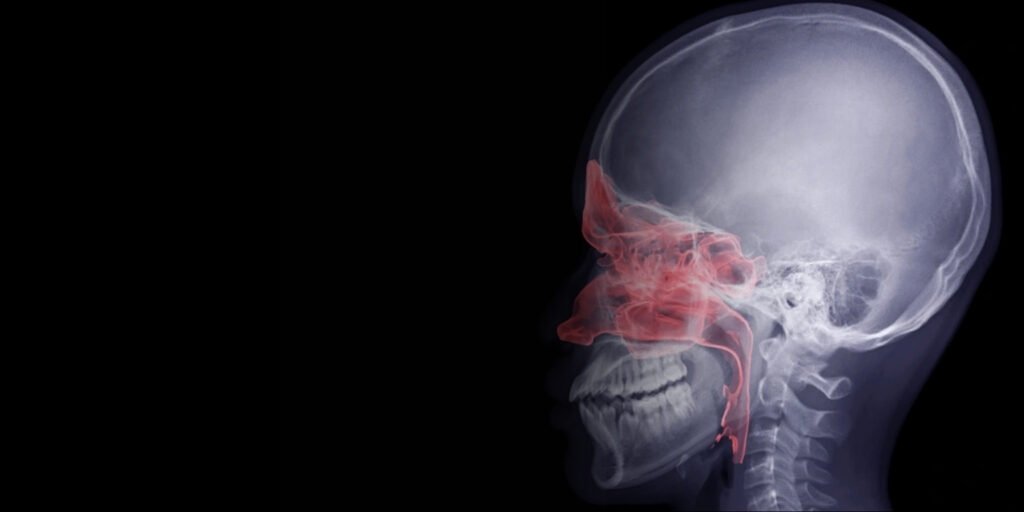
Skull base cancers are rare, complex tumors that grow at the bottom of the skull, involving critical areas such as the nasal cavity, sinuses, eyes, brain lining, and cranial nerves: their deep site and proximity to relevant structures make treatment very specialized in surgery and reconstruction.
Skull base cancers are rare, complex tumors that grow at the bottom of the skull, involving critical areas such as the nasal cavity, sinuses, eyes, brain lining, and cranial nerves: their deep site and proximity to relevant structures make treatment very specialized in surgery and reconstruction.
SKULL BASE CANCER
Signs & Symptoms
Skull base cancer develops at the bottom of the skull, affecting critical nerves and structures. Symptoms often appear gradually and may impact vision, hearing, and facial function.
Persistent Headaches
Continuous or worsening headaches caused by tumor pressure on the skull and brain structures.
Vision Changes
Blurred vision, double vision, or partial vision loss may occur due to optic nerve involvement.
Hearing Loss or Tinnitus
Tumors near the ear canal can cause hearing difficulties or ringing in the ears.
Facial Numbness or Weakness
Pressure on cranial nerves may lead to drooping, numbness, or muscle weakness.
Difficulty Swallowing or Speaking
Tumor growth can compress nerves affecting speech and swallowing.
Nosebleeds or Nasal Congestion
Tumors affecting sinuses may cause unexplained bleeding or chronic congestion.
SKULL BASE CANCER
CAUSES & RISK FACTORS
Skull base cancers can be caused by genetic, environmental, or medical factors. Awareness of risks helps in prevention and early detection.
Previous Radiation Exposure
Radiation to the head or neck may trigger abnormal cell growth in the skull base.
Genetic Mutations & Family History
Inherited syndromes can increase susceptibility to skull base tumors.
Chronic Infections or Inflammation
Long-term sinus, nasal, or ear infections may contribute to tumor development.
Age & Gender
Risk increases with age, though it can occur in younger individuals; some types are more common in men.
Weakened Immune System
Immunocompromised patients are more vulnerable to abnormal cell proliferation.
Lifestyle Factors
Smoking, alcohol use, and poor diet may indirectly affect susceptibility.
Treatment Options
Endoscopic Skull Base Surgery
Combined head & neck/neurosurgical procedure used for large or complex skull base tumors.
Neck Dissection
Microvascular Free Flap Reconstruction
Radiation/Chemoradiotherapy
Treatment Options

Endoscopic Skull Base Surgery
Open Craniofacial Resection
Neck Dissection
Microvascular Free Flap Reconstruction
Radiation/Chemoradiotherapy
Surgical Resection & Reconstruction
Skull base cancers often involve critical areas near the brain, eyes, nerves, and major blood vessels. Surgery in this region requires high precision, careful planning, and multidisciplinary expertise to achieve complete tumor removal while preserving vital functions.
Endoscopic Skull Base Surgery – A minimally invasive approach using nasal endoscopes to access and remove tumors at the skull base with minimal disruption to surrounding structures.
Open Craniofacial Resection – In advanced cases, tumors may require combined approaches through the skull and facial bones for complete clearance.
Segmental Bone Removal – If the tumor invades bone (such as sphenoid, temporal, or frontal bones), affected segments are removed to ensure safety.
Oncological Safety Margins – Surgeons focus on removing the tumor entirely while protecting critical nerves, vessels, and brain tissue.
Because skull base surgery can create significant structural and functional defects, reconstruction is key to restoring appearance, function, and protection.
Local Flaps – Small tissue flaps from nearby regions (nasal septum, turbinate mucosa, or pericranial flaps) can be used for limited defects.
Regional Flaps – Tissues from areas like the temporalis muscle or forehead are rotated to cover and protect exposed brain or nasal cavities.
Free Flaps (Microvascular Reconstruction) – For larger and complex defects, tissues from distant sites (thigh, forearm, or fibula bone) are transplanted with their blood supply to restore structure, separate brain from nasal passages, and maintain function.
Skull & Facial Bone Reconstruction – In some cases, grafts or prosthetic implants are used to rebuild bone defects and provide support.
Neurological Monitoring – Continuous follow-up is essential to assess brain function, vision, and cranial nerves.
Speech & Swallowing Therapy – Helps restore communication and swallowing if nerves or muscles are affected.
Cosmetic & Functional Recovery – Reconstruction ensures not only safety but also acceptable cosmetic outcomes, which improves quality of life.
Emotional Support – Skull base cancer surgery can be life-changing; psychological counseling and support groups help patients and families cope with recovery.
Why To Consult Dr. Natasha Lalwani?

Skull base cancers demand precision, planning, and perseverance. My goal is to remove the disease completely, rebuild what’s lost, and support you back to a confident, functional life.
~ DR. NATASHA LALWANI
Skull base cancers demand precision, planning, and perseverance. My goal is to remove the disease completely, rebuild what’s lost, and support you back to a confident, functional life.
~ DR. NATASHA LALWANI
Facing Skull Base Tumor Symptoms?
Early expert intervention dramatically improves outcomes.
Book your consultation with Dr. Natasha today for specialised skull base cancer care.